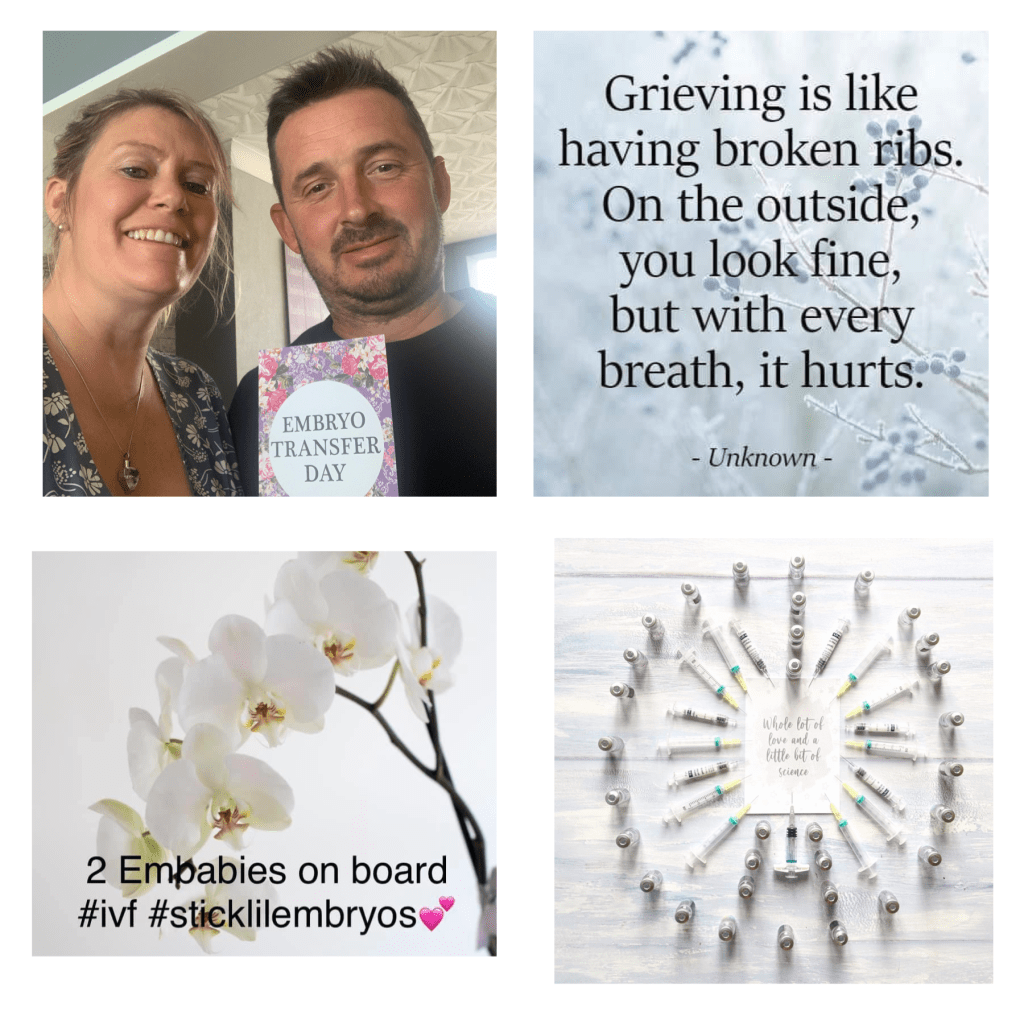
I often wonder if I should share as much as I have done online for anyone to access. I worry that my life is readily available for anyone to read about. Then I remind myself that it is only a part of my life I am sharing and the reason I do is to help others who are going through similar or know someone who is and to break the taboo subject of fertility, miscarriage, pregnancy loss, IVF and death of babies.
With that in mind I am writing today about our transfer. I will talk a little about exactly how it happens so if you are wanting to avoid images in your head that you might deem unpleasant then maybe now is a good time to stop reading.
The morning of our transfer Neil and I carried on with our day but it was clear that we were both anxiously waiting a phone call. We were hoping that we would not get a phone call as if we did it would be bad news and be telling us not to come for transfer as the embryos did not survive the thaw.
By the afternoon we were reassured as we did not have a phone call we were good to go for the transfer. Of course we did not know how many of our embryos had survived or made it from the night before to a grade they were happy to transfer.
Statistically only 5% of embryos don’t survive the thaw. Let’s say that there other way around in the positive way…95% of embryos survive the thaw.
As explained before we were having all 4 of our embryos thawed as they had not quite got to the blastocyst stage that the lab and doctors would have preferred.
Embryos are graded. The first 2 we had transferred in December 2019 were grade A. Top quality blastocysts! Our other 4 that have been frozen were deemed of a quality good enough to become a pregnancy.
I had a horrible feeling in my stomach that we would arrive and be told that 2 had not survived. You might wonder why as I often state we are positive people and the statistics are good for survival.
Throughout our fertility journey we have hit all the unlikely statistics! Only 1% of identical twins are MCMA. Only 2% chance of having a ectopic/heterotopic pregnancy when the woman doesn’t have any other underlining fertility conditions. Only 1 in 70,000 women don’t respond to the induction of labour and so on.
These are a few of the very unlikely statistics that Neil and I have fallen within. So it came as no surprise when the doctor informed us that one embryo did not survive the thaw and the other only got to grade D and would not make a viable pregnancy.
Neil and I have always stated that we would try 3 rounds of IVF if we could. We were elated when we got 6 embryos and knew this would fulfil our plan. However this round is now our last one as to undertake IVF again we would have to go back to the start of the process and undertake egg collection again costing about £8-10,000.
The doctor informed us that the other 2 embryos had made it to grade C and were good to be transferred. I know it is probably obvious but I’ll state it anyway grade C is not as good as grade A but remember they are good enough to make a viable pregnancy.
I step behind the curtain to remove my knickers and have that awkward moment where I can’t decide if I put them on the hooks provided, on top of the bin or on the floor. I decide to go with neatly folded on the floor.
For all those women that have had a smear the process of a transfer is similar. For all of those unaware of what that entails, you sit on a chair/bed with your legs spread apart and in supports.
The doctor then shines a light on your vagina and takes a piece of equipment that looks like a shut duck bill. He inserts this into your vagina and opens it whilst inside. It is then tightened to keep it exactly in place.
The lab technician then comes out with a very long stick/probe that holds on it the 2 embryos. The doctor then sticks this into the vagina and navigates to the place in the womb where he wants to position them with the help of a nurse using an ultrasound. It is uncomfortable but otherwise pain free.
The probe/stick is then given back to the lab technician to check that there are no embryos left on it. In our case we got the thumbs up. A ultrasound image is then printed which shows a white dot in the woman’s womb this is the embryos aged 6 days old in our case.
The process itself takes about 5 minutes. The difference this time round for us is the embryos are lower and have been glued. This is the term they use in relation to making them sticky. This is now standard procedure in our clinic. When we had our last transfer the embryos were not glued.
So what happens now? We are now in what is known as the two week wait. The embryos will implant over the next few days if they are going to and this would result in a positive pregnancy test. If they don’t implant then I will have my period the same as I would naturally after unsuccessful ovulation.
The two week wait is considered the hardest part of IVF (it’s all hard if you ask us) as now you just have to wait and your hormones and emotions are tested daily. You question every twinge and don’t know if that pain was possibly an implanting pain or are your boobs sore from the medication or are you pregnant?
We have undertook a two week wait previously and we didn’t get to our official test day as I bleed before it arrived. Of course we know now that I was pregnant with twins but one was in my tube. So even if I bleed this time we are taking a test!
Last time Neil and I coped well with the two week wait. The only medication we had to continue was pessaries. This time I have to continue to take the tablets, pessaries and injections. This is because it is a frozen cycle and not necessarily in line with my body’s cycle so science has to take over.
The medication will continue up to the official test date and we will then be advised if we need to continue anything. We already know that if we get a positive then we are to continue the pessaries until 16 weeks pregnant.
I am now to rest for the next few days and give my body the chance to relax and allow the embryos to implant. No dog walking, housework or other activities for me (there is a plus side to all of this)!
I am feeling very emotional. My eyes filled with tears when we were told that two embryos didn’t make it. I am they kind of person that needs a plan and hope. It means that this cycle is our last chance. I’m not sure I’m ready for this to be our last chance.
I know that this cycle might be successful and therefore we don’t need to be worrying about more chances. It is however very hard to feel unnerved when our four pregnancies have resulted in loss. We not only need a positive but we need to get through a whole pregnancy.
It didn’t help that I got the time of the procedure wrong and coming home took hours as we were stuck in traffic due to a car fire on the motorway. Not quite the relaxing that the doctor ordered but stayed calm and just sat there so no harm done.
I had also asked to not be informed about the grades as I consider them to be irrelevant. On the forums you see lots of women becoming pregnant from lower graded embryos. Neil and I spoke about this and also told ourselves that the glue must be an additional positive factor.
If we reach our test day and get a positive we will be scanned in 4-5 weeks (5-6 weeks pregnant). This scan will tell us if we have 1 baby or 2. It will tell us if the position is correct (ie not in my tube). We won’t know if any baby has a heartbeat until just over 6 weeks pregnant.
I guess we are in a very different place from being naively pregnant for the first time. With everything we have endured it is understandable that we are realistic about our fertility and IVF. This is not to say that we are not also optimistic we just know that it’s not as easy as just positive or negative.